
Hepatic encephalopathy affects young cats more often than old cats. AC Manley / Shutterstock.com
Hepatic encephalopathy refers to a collection of neurologic changes that occur when the liver doesn’t filter out certain toxins in the blood. This condition is fortunately uncommon in cats, but if your cat recently received this diagnosis, you might be wondering how serious it is and what kinds of treatments are available.
In this article, you’ll learn about what causes hepatic encephalopathy in cats, how to recognize it, and the ways to treat it.
What Is Hepatic Encephalopathy?
“Hepatic” means liver and “encephalopathy” refers to a disease affecting the brain. Together, these words define a collection of observed neurologic symptoms that occur when toxins build up in the brain. This happens if the liver, responsible for removing toxins from the bloodstream, is not functioning properly or if the toxins bypass the liver.
Where do toxins come from, you might be wondering. They can form after a breakdown of normal processes in the body. For example, ammonia—a highly toxic compound—forms when protein is broken down in the gastrointestinal tract. Ammonia produced during digestion usually goes directly to the liver to be converted into a harmless substance.
But if the liver is not working right, or if ammonia can bypass the liver’s processing, it can reach toxic levels in the body that can harm the brain.
Hepatic encephalopathy is not just a cat disease. It can occur in dogs, humans, and other animals. Cats can be mildly affected or have a severe case, sometimes resulting in death. Fortunately, hepatic encephalopathy is uncommon in cats.
Causes of Hepatic Encephalopathy in Cats
There are several potential causes of hepatic encephalopathy in cats.
Portosystemic Shunts
A portosystemic shunt (PSS), also known as a liver shunt, is a blood vessel that inappropriately allows blood to go around the liver instead of through it, which means it won’t go through the liver’s detoxification process. This is considered the most common cause of hepatic encephalopathy in all animals, including cats.
A congenital portosystemic shunt is a shunt that cats are born with. An animal might also develop one or more shunting vessels secondary to chronic liver disease and some other conditions (acquired portosystemic shunt).
Congenital shunts are much more common in cats, and signs are usually seen in younger cats. Some cat breeds might be at higher risk, including Siamese, Himalayans, Burmese, and Persians.
Hepatic Lipidosis
Also called fatty liver disease, hepatic lipidosis is the second most common cause of hepatic encephalopathy in cats. Hepatic lipidosis occurs when a cat (especially an overweight or obese cat) stops eating abruptly. Within as soon as 24 hours, fat stores are mobilized in the body, accumulating in the liver. Overwhelmed by this process, the liver no longer functions properly.
Acute Liver Failure
Acute liver failure is less common. Causes of acute liver failure most often include a toxin ingestion (such as acetaminophen/Tylenol), a severe infectious or inflammatory process, or trauma.
Chronic Inflammatory Liver Disease
Hepatic encephalopathy is a rare side effect of a common feline chronic disease of the liver and bile ducts called cholangitis/cholangiohepatitis syndrome, or CCHS. There can be many causes of CCHS, including infection, chronic inflammatory disease (especially alongside chronic pancreatitis and/or inflammatory bowel disease), and cancer. The development of hepatic encephalopathy might depend on how severe the disease is and how much liver function has been lost over time.
Classification of Hepatic Encephalopathy in Cats

Icterus or jaundice, a yellowing of the skin, is one sign of liver disease like hepatic encephalopathy in cats. Todorean-Gabriel / Shutterstock.com
Hepatic encephalopathy is classified in two ways. The first classification is based on what is causing the disease:
- Type A: Caused by acute liver failure.
- Type B: Caused by portosystemic shunting of blood.
- Type C: Caused by cirrhosis (chronic liver failure), which combines acquired shunting and poor liver function together.
The second classification is based on the severity of symptoms:
- Grade 1 (mild): Mild lethargy (low energy) and signs of disorientation or confusion.
- Grade 2 (moderate): Increased lethargy, personality changes, mild wobbliness when walking, and inappropriate behavior (house soiling or altered social behavior like signs of fear or aggression).
- Grade 3 (advanced): Worsening signs of wobbliness when trying to walk (ataxia), confusion, excessive drooling, (temporary) loss of vision, walking in circles, pressing the head into a wall, significant personality changes, and worsening drowsiness.
- Grade 4 (severe): Minimally or unresponsive to stimulation, significant mental dullness or lethargy, seizures, and coma. Cats showing these signs have a high risk for impending death.
The grade typically depends on the underlying disease. For example, a Grade 4 case, which is the most severe, is often caused by acute liver failure or trauma.
The presence of portosystemic shunts or chronic disease more often will contribute to the other three grades. Disease not recognized early enough might progress into the higher grades of disease.
Symptoms of Hepatic Encephalopathy in Cats
For symptoms of hepatic encephalopathy to be seen, approximately 70% of liver function must be lost. Alternatively, one or more portosystemic shunt vessels must be present.
In addition to the symptoms in each grade, other signs that might be seen with advanced liver disease in cats can include:
- Icterus/jaundice (yellowing of the eyes, skin, and gums)
- Poor appetite
- Vomiting
- Diarrhea
- Weight loss
Complications of Hepatic Encephalopathy in Cats
If hepatic encephalopathy comes on acutely or goes undiagnosed for a long time, complications can be severe and life-threatening.
In these acute or severe cases, other toxic products as well as ammonia build up to the point that dangerous swelling of the brain can occur (cerebral edema). This is often the case in cats that are showing signs of coma or seizures.
Diagnosis of Hepatic Encephalopathy in Cats
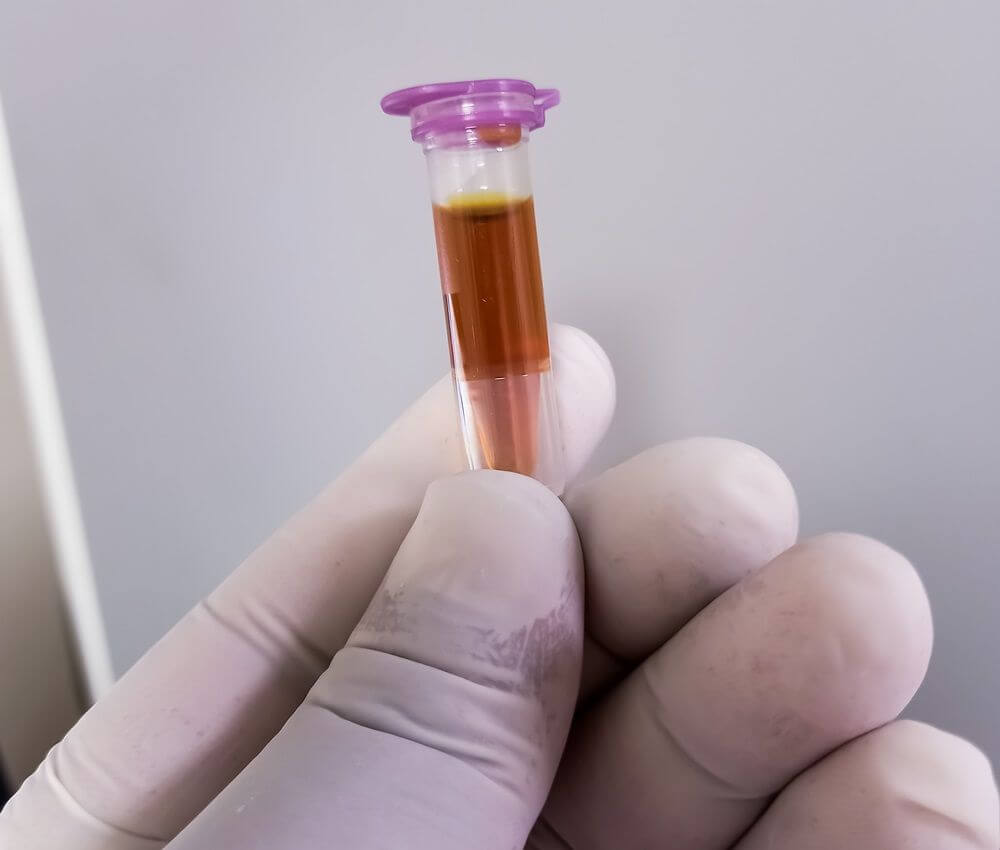
lf a cat has hepatic encephalopathy, their blood serum might have an abnormal yellow or brown color. Babul Hosen / Shutterstock.com
Before diagnosing, your cat’s vet will conduct a physical examination and collect medical information. If you report symptoms of hepatic encephalopathy, the vet will likely examine your cat for neurologic disease or signs of liver failure.
When it comes to their health, cats can be real puzzles—if only they could tell us what’s wrong. Instead, because some symptoms are shared among diseases, your vet might recommend additional testing to confirm the diagnosis.
Bloodwork
Your vet might order bloodwork to check:
- Alanine aminotransferase, a primary liver enzyme
- Alkaline phosphatase
- Bilirubin, a yellow pigment that, when elevated, causes signs of jaundice
- Blood glucose
Bile Acid Testing
This is a type of bloodwork that specifically assesses the liver’s ability to handle ammonia and is the supportive test of choice to screen for a portosystemic shunt.
Blood Clotting/Coagulation Testing
One other function of the liver is to produce certain factors that allow blood to clot normally. This testing may be advised to support a diagnosis of liver failure, or if there is a concern about bleeding.
Urinalysis
A urine dipstick can test for bilirubin in the urine. Bilirubin in the urine indicates that it has built up in the bloodstream due to a liver or bile flow problem.
Ultrasound
This is the test of choice to look for portosystemic shunts. There are a few different kinds and locations for these aberrant vessels. Ultrasound can be used to directly see blood vessels and where blood flow is being rerouted. Ultrasound is also very helpful for viewing the liver tissue itself and collecting cell and tissue samples that can help with diagnosis.
CT and MRI
Computed tomography (CT) and magnetic resonance imaging (MRI) are advanced imaging techniques used to look for portosystemic shunt vessels as well, especially if the vessels cannot be identified well with ultrasound. These techniques can also be used to check for other causes of neurologic disease in the brain and spinal cord.
X-Ray
X-rays are of limited use in diagnosing specific liver disease, but might help in identifying abnormal liver size or a large tumor, and for ruling out other causes of a cat’s symptoms.
Treatments for Hepatic Encephalopathy in Cats

Helping an overweight cat lose weight might reduce the risk of hepatic lipidosis (fatty liver disease), which is one cause of hepatic encephalopathy in cats. Andriy Blokhin / Shutterstock.com
Treatment for hepatic encephalopathy in cats depends on the cause and severity.
Whatever the cause, very severe Grade 4 disease must be treated immediately at a veterinary hospital capable of seeing advanced emergency cases. Emergency treatment must be given to quickly reduce fluid swelling around the brain and treat actively seizing patients.
Milder cases of hepatic encephalopathy can be managed medically. The following treatments focus on reducing ammonia levels throughout the body.
- Lactulose: Also used as a laxative, lactulose in this case is used for its ability to pull ammonia out of the bloodstream and into the colon where it can be excreted.
- Reduced dietary protein: Prescription diets, such as the Hill’s l/d diet or Royal Canin Renal Support diet, have more moderate levels of dietary protein that are also more highly digestible. Restricting protein to very low levels is not appropriate as these cats still have high needs for protein. Dietary protein changes are not necessary in all cases but can help reduce how much ammonia gets produced in the digestive tract from protein breakdown.
- Antibiotics: Lower doses of metronidazole can be used to reduce the number of ammonia-producing bacteria in the gastrointestinal tract. Although long-term antibiotic use is not ideal, this strategy might be needed if a cat’s condition responds well.
- Liver supplements: Depending on the underlying nature of liver disease that is present, liver supplements containing S-adenosyl methionine (SAMe) and milk thistle (Denamarin), and others might be recommended to help support liver health.
- Surgery: In the case of a portosystemic shunt, surgery might be an option. If the shunting vessel can be identified, it can be closed surgically so that blood flow from the gastrointestinal tract is no longer bypassing the liver. This can be a very successful option in many cases, especially if a diagnosis is made early.
Cat Care Tips
Here are a few things to keep in mind regarding hepatic encephalopathy in cats:
- Young cats are at the highest risk for portosystemic shunts. Signs of poor growth and progressive neurologic changes in a young cat should be investigated as soon as possible.
- Overweight cats are at higher risk, but any cat can develop hepatic lipidosis from sudden loss of appetite. If your cat suddenly stops eating, don’t wait more than 24 hours to see a veterinarian.
- In most cases, hepatic encephalopathy is the result of chronic progression. Annual exams and wellness monitoring lab work can be helpful for an early diagnosis.
- Never give your cat human medications as some might cause liver toxicity (acetaminophen).
Prevention of Hepatic Encephalopathy in Cats
One of the most preventable causes of hepatic encephalopathy is toxin ingestion or trauma. See the ASPCA Animal Poison Control website for a comprehensive list of toxic plants, foods, and household products (including human medications) so you can keep them out of your cat’s reach.
Cats with portosystemic shunts are most often born with them. Early recognition and diagnosis are key.
Chronic liver disease in cats is an uncommon cause of hepatic encephalopathy, but early detection with wellness monitoring once or twice a year is helpful. If therapies to treat underlying liver disease are started sooner, hepatic encephalopathy is less likely, and severe disease can be prevented.
-
Williams, K. Hepatic Encephalopathy. VCA Animal Hospitals.
-
Center, S.A. (2023, August 10). Hepatic encephalopathy in small animals. Merck Veterinary Manual.
-
Brister, J. Hepatic Encephalopathy in Dogs and Cats. Veterinary Partner.
-
Twedt, D.C. Hepatic Encephalopathy—Feline. Purina Vet Center.
-
Lidbury, J.A., Cook, A.K., & Steiner, J.M. (2016). Hepatic encephalopathy in dogs and cats. Journal of Veterinary Emergency and Critical Care, 26(4), 471–487.
-
Dacvim, A.C.K.D. (2020, April 27). Feline liver disease (Proceedings). DVM 360.
-
Choi, J., & Kim, J. (2023, May 1). Feline hyperammonemia associated with functional cobalamin deficiency: A case report. PubMed Central (PMC).
-
Konstantinidis, A.O., Patsikas, M.N., Papazoglou, L.G., & Adamama-Moraitou, K.K. (2023). Congenital portosystemic shunts in dogs and cats: Classification, pathophysiology, clinical presentation and diagnosis. Veterinary Sciences, 10(2), 160.
-
Portosystemic shunt. (n.d.). Cornell University College of Veterinary Medicine.







